"Muhammad," a 42-year-old pseudonym, experienced a profound psychological upheaval following the passing of his mother, a loss that deeply impacted him. Struggling to readjust to both his social and familial spheres, he found himself grappling with grief, spending his nights in tears as he reminisced about the woman, he had devoted his life to caring for. Reluctant to seek professional help from a psychiatrist due to fears of societal stigma and potential embarrassment among friends, he instead turned to a friend working in the spiritual realm. Exploring herbal remedies in search of solace, he persisted in this alternative approach for approximately three months, foregoing traditional psychiatric intervention.
Muhammad was assigned to work in the Sulaymaniyah Governorate, tasked with attending seminars and developmental workshops as part of his duties. During one such workshop, which emphasized psychological support, he seized the opportunity to privately engage with the psychiatrist conducting the session. Feeling a sense of anonymity among the attendees, Muhammad approached the psychiatrist, pouring out his emotional turmoil in tears within the confines of an isolated room. There, he received invaluable guidance on how to address and alleviate his psychological distress.
He maintained regular communication with the psychiatrist for several months, during which time his condition gradually stabilized. However, he still required occasional phone consultations to address any lingering psychological issues.
"Asma," a 33-year-old alias, grapples with significant psychological pressures stemming from her husband's financial troubles. She confided in The New Region, explaining that her husband had borrowed substantial sums of money that she was now responsible for repaying. This burden weighed heavily on her, causing extreme worry and insecurity not only in her professional life but also within her social circles.
Initially, Asma sought solace from a spiritual healer, engaging in recitations of specific prayers and using herbal remedies containing Quranic verses, which provided temporary relief. However, the stress and psychological anxiety persisted, prompting her to consider professional psychiatric help. Living in Nasiriyah, where psychiatrists were scarce and societal judgment loomed large, she hesitated to seek traditional therapy. Instead, she opted for phone consultations with a psychiatrist, explaining that her prominent family background made her wary of being seen seeking mental health treatment. Only two trusted friends were privy to these confidential calls.
Ahmed Hassan Beyan, the dean of the medical college at Sumer University and a practicing psychiatrist, shed light on the pervasive societal stigma surrounding mental health care in Iraq. Speaking to The New Region, he underscored how this stigma dissuades medical students from pursuing psychiatry as a specialization, contributing to the scarcity of psychiatrists not only in the province but across the country.
Dr. Beyan elaborated on the challenges faced by aspiring psychiatrists, highlighting the academic rigor required to study psychiatry as a scientific discipline. Despite this, the field offers fewer financial incentives compared to other medical specialties, further deterring potential candidates. This disparity in financial returns post-graduation exacerbates the shortage of psychiatrists in Iraq, perpetuating the systemic inadequacy of mental healthcare.
In response to prevailing societal stigma, Dr. Beyan opted to conduct online sessions to connect with certain psychiatric patients for a period. While acknowledging that the effectiveness of these sessions falls short of desired levels, he emphasized the necessity of such measures given the prevailing circumstances.
Dr. Ibrahim Safaa Al-Sa'igh, the director of the Mental Health Office at Thi Qar Health Directorate, disclosed to The New Region that despite a population exceeding two million and 380 thousand inhabitants, the province only boasts four psychiatrists. This starkly falls short of the global standard, which recommends one psychiatrist for every 10,000 citizens. With this benchmark in mind, currently there's approximately one psychiatrist for every 600,000 people, highlighting a glaring disparity in mental health resources.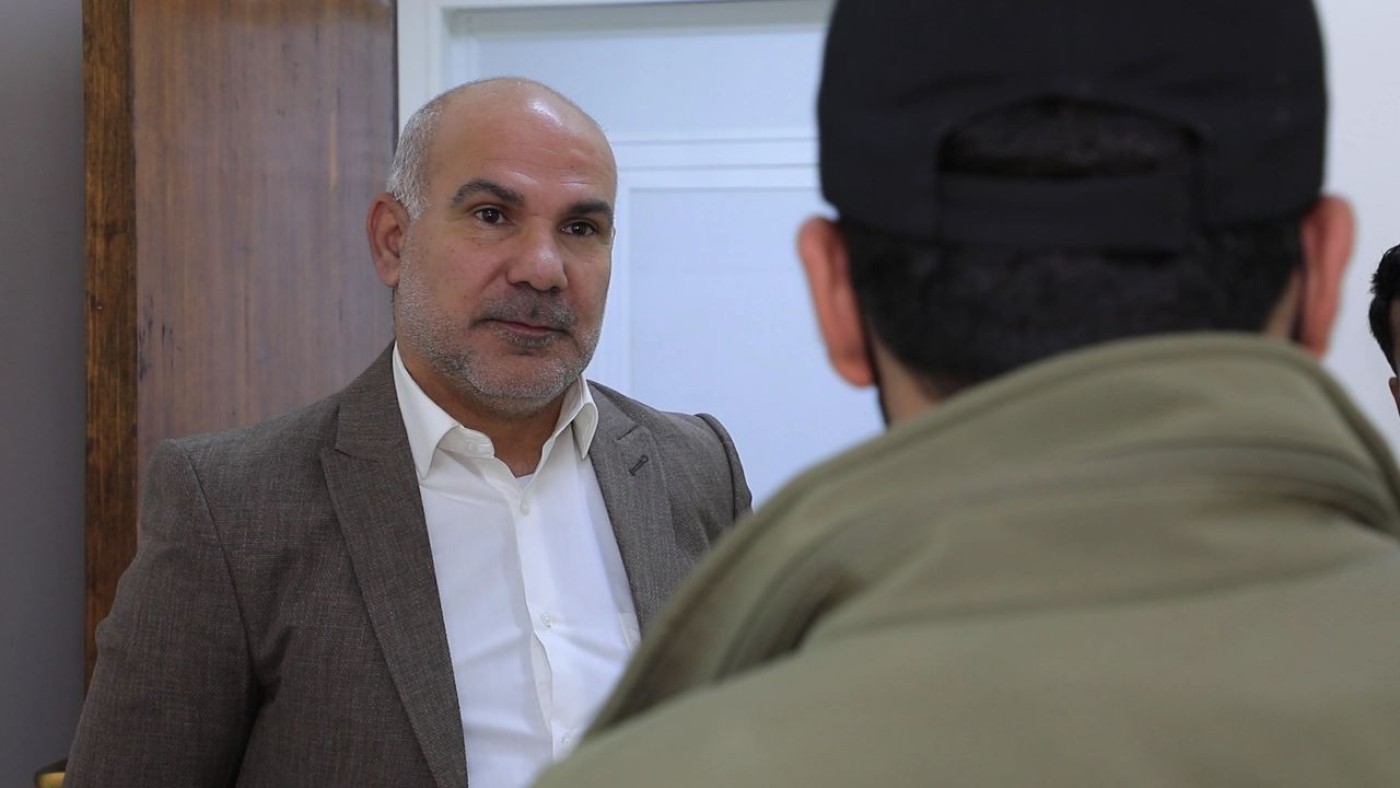
According to al-Sa'igh, the psychiatrist's role extends beyond treating mental disorders to addressing drug addiction, a pressing issue given the escalating number of users. Consequently, there's a call for heightened governmental support for psychiatrists and initiatives to incentivize medical students to pursue this specialized field.
In 2022, the government-run Life Recovery Center saw 803 visits from drug addicts and 1294 from patients with mental disorders. However, in 2023, the number of drug addicts seeking help surged to 1406, while the count for mental disorder patients slightly decreased to 1308.
Al-Sa'igh notes a shift in public perception towards psychiatric treatment, attributing it to heightened awareness. Individuals now view those with mental conditions as patients deserving of treatment. However, certain barriers persist, as many patients still take precautions like wearing masks and hats when visiting medical facilities to evade recognition by acquaintances.
Salah Al-Mousawi, the director of the Southern Studies and Planning Center, asserts that since 2003, Iraq has experienced heightened levels of conflict, including wars, armed confrontations, and psychological issues stemming from various factors. These include the presence of American forces, subsequent terrorist activities by organizations like Al-Qaeda and ISIS, and the COVID-19 pandemic. These challenges have led to increased instances of psychological problems such as panic, anxiety, and depression, as well as rising rates of drug abuse, unemployment, and suicides. Al-Mousawi emphasizes the urgent need for a national strategy to address these healthcare deficiencies.
Dr. Saif Al-Badr, the spokesperson for the Ministry of Health, disclosed in a press statement the alarming increase in suicide rates across Iraq from 2017 to 2022, with a variety of methods being employed. He identified psychological factors as the primary cause, compounded by social, familial, and economic pressures, as well as substance abuse.
The World Health Organization has previously highlighted that one in every four Iraqis grapples with mental fragility, against a backdrop of just three psychiatrists per million people in the country. This reality is rooted in worsening psychological well-being, compounded by factors such as domestic violence, the aftermath of war, and economic crises.
Hayder Al-Maliki, the president of the Iraqi Psychiatric Association, revealed to The New Region that there are currently 209 psychiatrists practicing in Iraq, with 45 of them located in the Kurdistan Region. Each year, there is a modest increase of approximately 12 to 20 psychiatrists entering the profession to bolster healthcare services. This uptick can be attributed to incentives offered by the Ministry of Health, which include waiving old residency conditions and GPA requirements for psychiatrists and exempting them from mandatory service in rural areas.
Al-Maliki highlights an uptick in patient referrals to psychiatrists, albeit gradual, which he attributes to shifting attitudes toward mental health. There's a growing recognition that individuals grappling with mental health issues are patients in need of care, rather than being unfairly stigmatized as "insane" as was once the prevailing perception.



 Facebook
Facebook
 LinkedIn
LinkedIn
 Telegram
Telegram
 X
X


